Epidemic Diseases of the Great Famine
Published in 18th–19th - Century History, Features, Issue 1 (Spring 1996), The Famine, Volume 4 Famine can be defined as a failure of food production or distribution, resulting in dramatically increased mortality. In Ireland between 1845 and 1849, general starvation and disease were responsible for more than 1,000,000 excess deaths, most of them attributable to fever, dysentery and smallpox. These three highly contagious diseases, which had long been endemic in Ireland, swept the country epidemically and with great malignity during these years. Their destructiveness was intensified by the presence of other epidemic infections, especially tuberculosis, bronchitis, influenza, pneumonia, diarrhoea and measles. The arrival of Asiatic cholera as a pandemic in 1848-49 exacerbated the situation. This fearsome disease added to the physical and mental suffering of the beleaguered population and increased the overall mortality.
Famine can be defined as a failure of food production or distribution, resulting in dramatically increased mortality. In Ireland between 1845 and 1849, general starvation and disease were responsible for more than 1,000,000 excess deaths, most of them attributable to fever, dysentery and smallpox. These three highly contagious diseases, which had long been endemic in Ireland, swept the country epidemically and with great malignity during these years. Their destructiveness was intensified by the presence of other epidemic infections, especially tuberculosis, bronchitis, influenza, pneumonia, diarrhoea and measles. The arrival of Asiatic cholera as a pandemic in 1848-49 exacerbated the situation. This fearsome disease added to the physical and mental suffering of the beleaguered population and increased the overall mortality.
 |
Fever
Fever appears to have been a feature of the country for hundreds of years. Twelfth-century visitors commented on its extent and prevalence, as did Gerald Boate, during the Cromwellian wars. Boate called it ‘malignant fever’ and said it was ‘commonly accompanied with a great pain in the head and in all the bones, great weakness, drought, loss of all manner of appetite, and want of sleep, and for the most part idleness or raving, and restlessness or tossings, but no very great nor constant heal’. In later centuries, fever was variously described as the country’s ‘scourge and chief destroyer’, its ‘great element of destruction’ for hundreds of years. Eighteenth and nineteenth-century doctors did not know how the disease originated. Some contended that famine was the sole or paramount cause, others that food shortage was only one of several possible precipitating factors. Among the latter were poverty, the wretched housing of the poor, the paucity and inferior quality of their diet, their lack of clothing and fuel, dirt, depression, and intoxication, not to mention the pig in the kitchen and the middens that disgraced the frontage of every cabin in the country.
Some Irish medical practitioners traced the country’s recurring outbreaks of fever to some unknown connection between atmospheric or electrical phenomena and the generation of disease, the so-called ‘epidemic constitution’. This was entirely beyond the power of man to control or even comprehend properly. According to the distinguished Dublin physician and teacher, Robert J. Graves, the ‘epidemic constitution’ was some general atmospheric change that affected the whole island simultaneously. The definitions offered by his colleagues were equally vague. To one, it was an influence in the air, an unspecified ‘something’, to another the ‘epidemic constitution’ was ‘some potent aerial poison’. One of the few specific explanations offered was that of a King’s County medical practitioner who attributed an outbreak of fever at Aghamon in November 1848 to an aurora borealis which, he claimed, had shone with great brilliancy over the entire district.
Typhus
It is now known that the vector of fever was not famine, nor social distress, still less atmospheric abnormalities, but pediculus humanus, the human body louse. It is also known that there were two distinct but symptomatically related infections involved, typhus fever and relapsing fever. The typhus infection can enter the body through scratches on the skin, through the conjunctiva (?), or by inhalation, while relapsing fever is generally contracted through the skin. Typhus symptoms include high fever, prostration, mental confusion, body aches and a characteristic rash which covers the trunk and limbs of the body. In cases which are not going to recover, death usually occurs from heart failure about the fourteenth day. High temperature, generalised aches and pains, nausea, vomiting, nose bleeding and jaundice are features of relapsing fever. In cases with a favourable outcome, the fever ends after five or six days with a sharp crisis attended by profuse sweating and exhaustion. This drop in body temperature was colloquially known as ‘getting the cool’. The symptoms return after about a week and there may be several such relapses before the disease runs its course.
During the Great Famine, relapsing fever was the prevalent disease among the general population, while the higher social classes tended to contract the more deadly typhus fever, especially those who were most exposed to infection, notably clergymen, doctors, members of relief committees and those connected with the administration of the poor law. The mortality rate from typhus was also more pronounced among the middle and upper classes than it was among the poor, who may have developed some immunity through long-term exposure.

Mullins’ hut at Scull, by James Mahony, ARHA. The visitor was the Revd. Dr Robert Traill, The local vicar, who succmbed to fever shortly after.
(Illustrated London News)
Optimum conditions for lice infestation
The relationship between famine and fever is complex, but there is no direct nutritional connection. Increased vagrancy and mendicity, as well as overcrowding and the neglect of personal and domestic hygiene, all of them features of famine, created the optimum social conditions for lice infestation. In Ireland, in the late 1840s, infected lice feasted on the unwashed and susceptible skin of the hungry, multiplied in their filthy and tattered clothing, and went forth, carried the length and breadth of the country by a population who had taken to the roads, vagrants and beggars, as well as the evicted and those who had abandoned their homes voluntarily. Lice found new and unresisting hosts at food depots and relief works, at social and religious gatherings, and in many public institutions, such as prisons and workhouses.
Reports from various parts of the country suggest that the first stage of the prevailing ‘famine fever’ was relatively mild. An account from Inishboffin stated that the initial attack was so slight that the afflicted ‘walked or rather staggered about with it’, while a Dublin doctor related that many passed through the fever ‘while they were literally walking about’. A characteristic of ‘famine fever’ was the voracious hunger displayed by the patient after the attack had ended. ‘The hunger was in their hearts’, said a nurse from the Queen’s County. When the relapse occurred, it was invariably more prolonged and severe. A County Limerick doctor reported that ‘the relapsed stage was long, from ten to fourteen days, very severe, attended with great debility and prostration of strength’. These recurring bouts of fever further weakened an already debilitated population and left them very vulnerable to a host of other infections, notably dysentery and diarrhoea.
Dysentery
The term ‘dysentery’ was formerly applied to any condition in which inflammation of the colon was associated with the frequent passage of bloody stools. The term is now restricted to amoebic dysentery, which is almost entirely confined to tropical and sub-tropical countries, and to bacillary dysentery, an infectious disease which may occur sporadically or in epidemics. The disease is caused by the dysentery bacillus and the infection is spread by flies, by direct contact, or by pollution of the water by faeces infected with the bacillus. Symptoms vary from a mild attack of diarrhoea to an acute fulminating infection. The duration of the diarrhoea varies from a few days to a fortnight, depending upon the severity of the attack. There may also be nausea, aching pain in the limbs, and shivery feelings, while there is always fever. An attack cannot develop except through the agency of the specific bacillus. However, anything which causes an intestinal upset, such as unsuitable food, predisposes to infection. Dysentery is rendered more virulent by famine and by the concurrence of other exhausting diseases.
During the terrible winter of 1846-47, chronic dysentery, or ‘starvation dysentery’ as it was sometimes called, was reported to be very prevalent among the destitute. In west Cork, which was one of the worst famine affected areas of the country, one doctor noted that the pulse of those suffering from this horrible affliction was almost entirely absent, that the extremities of the body were livid and cold, the face haggard and ghost-like, the voice barely audible and reminiscent of the cholera whine. The smell from evacuations was very offensive, almost intolerable, he said, and was similar to that of ‘putrid flesh in hot weather’. The discharges continued unabated until the body wasted to a skeleton. One Cork city doctor commented on the ‘loathsome, putrid smell’ that surrounded the diseased, as if, he said, ‘the decomposition of the vital organs had anticipated death’.

Lithograph by A. MacLure, from Lord Dufferin and Hon G.F. Boyle, Narrative of a journey from Oxford to Skibbreen…. 1847
Smallpox
Smallpox, which appeared epidemically in a very malignant form during the Great Famine, is no longer an active infection. It was an acute viral disease which was generally transmitted by airborne droplets. The characteristics of smallpox were high fever, headache, pain in the back and muscles, and occasionally in children vomiting and convulsions. In the severest infections, extreme toxaemia and massive haemorrhaging into the skin, lungs and other organs could cause death very quickly. In most cases, the afflicted survived to experience the characteristic rash two to five days after onset. Shortly afterwards, the small pimples of the rash turned to pustules, the drying and crusting of which began on the eight or ninth day after the first eruptions. The scabs fell off three or four weeks after the commencement of the disease, leaving the victim invariably with a pocked and scarred face. Blindness was a possible consequence, as was infertility in males.
Infectious diseases, such as fever, dysentery and smallpox, terrified the poor, and with good reason. Such afflictions pauperised, when they did not kill, and reduced the most vulnerable and oppressed to squalid misery and despair. Fever had a devastating impact on the already precarious existence of the poor. Each attack, with the weakness it left behind, lasted about six weeks and, with successive family members being struck down, fever might persist in a poor man’s cabin for months on end. Convalescence was slow and tedious, often taking six weeks and more, by which time a wage-earner’s family could be reduced to absolute poverty. Illness drove the poor into the pawn shops or compelled them to sell their meagre possessions, a pig, a cow, their miserable household furniture, or reduced them to the ultimate degradation, begging in public.
(Report of the Commissioners of Health, Ireland, on the epidemics of 1846-50).
Fever hospitals
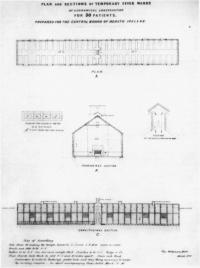
The fear of infection and the general acceptance of the contagiousness of fever and other epidemic diseases led to the establishment of special hospitals for the isolation of the infected. Three different types of institutions, county, district and poor law union fever hospitals, evolved during the first half of the nineteenth century. The poor law union fever hospitals were the most recent, dating from 1843. They were supported out of the rates and were open to all who resided within the poor law union. County fever hospitals, which admitted the infected from all parts of the county, were entirely supported by local taxation. They evolved fitfully and by the time of the Famine not every county had one. District fever hospitals, which dated from the 1816-1819 fever epidemic, were supported by a combination of local philanthropy and local rates. Unlike county fever hospitals, there was no limit to the number which could be established. However, their method of funding, not least the necessity of raising local subscriptions on an annual basis, retarded their development. At the commencement of the Famine, there were about a hundred permanent fever hospitals in the country.
Additional accommodation was provided for the infected in wooden sheds and tents, which were often pitched in the grounds of existing hospitals. In those parts of the country where there were no medical institutions of any description, the sick, when not abandoned to their own devises, were isolated as far as possible at home or quarantined in so-called ‘fever huts’. These were wretched structures of mud or stone which were hastily thrown up at the side of a road, the corner of a field, or the verge of a bog. Some were even more rudimentary, consisting of nothing more than straw and furze tied together and placed at an angle to the ditch. In these primitive shelters, the hapless, isolated victims of fever, struggled with cold and damp, hunger and thirst, as well as infection, totally dependent on the benevolence of others and the vagaries of fate.

A later artist’s impression of people seeking admission to an Irish workhouse during the Famine, from Robert Wilson, The life and times of Queen Victoria(London 1887-88)
Domestic quarantine, which was variously inspired by family affection, the absence of hospitals or the fear of entering them, was also a feature, one which was resorted to by rich and poor alike, although one pre-Famine report from County Kilkenny suggests that it was the class of ‘comfortable farmers’ who were most likely to resort to the practice. In single-roomed dwellings, those afflicted with fever were placed at one end of the cabin, while the healthy attempted to ward off infection as best they could at the other. In more substantial dwellings, the practice was to isolate the sick in a room by blocking up the door with sods. A hole was made in the rear wall, through which the medical attendant had to scramble on all fours. Some doctors blamed the very high rate of mortality from fever among their colleagues on having to spend so much time in what one of them called ‘the wretched cabins of the poor’. The popular attitude to fever hospitals was often ambiguous. There was a widespread suspicion that these institutions were sources of infection, a suspicion which hardened during the Great Famine when 373 emergency institutions were added to the hundred or so fever hospitals already in existence. The presence of a temporary fever hospital in a district, or the proposal to establish one, often provoked a very powerful response. For instance, an attempt by the famine relief committee in Clonakilty, County Cork, to open such an institution at the beginning of 1846 was thwarted by the general refusal to rent premises to them, either in or outside the town. It appears that the merest rumour of their intention was sufficient to cause a panic wherever they went. Similarly, a poor law inspector reported from County Kerry in June 1847 that it was impossible to procure a house for use as a fever hospital in any small town in the Killarney union. ‘The inhabitants positively refuse it through apprehension of fever’, he said.
In December 1846, the board of health in Drumkeeran, County Leitrim, resolved to hire a house for use as a fever hospital, there being no such institution within a radius of eighteen miles. The proposal caused ‘inconceivable alarm’ in the town. Sixty-two of the residents, including merchants, shopkeepers, tradesmen, labourers, publicans, and householders, as well as Pat Gallaher, the schoolmaster, addressed a memorial to the Lord Lieutenant, objecting to the establishment of a fever hospital in the centre of the town. They stated that they were not so much opposed to the institution, as to its location. The lay-out of the town was such that fever patients would have to be transported through the main street, a necessity which they maintained posed an unacceptable risk to the town’s 600 inhabitants and to visitors on market day and fair day. They were also concerned about the threat to the commerce and trade of the entire locality. The appellants urged the Lord Lieutenant to protect their families and themselves from what they termed ‘an immediate exposure to plague’, by directing that the proposed hospital be established outside the town.
A rather similar appeal was made by the residents of Kinvarra, County Galway, in July 1847. They claimed that the imminent opening of a fever hospital in the town placed their lives and those of their families in ‘the greatest peril’. They argued that the chosen site was too close to the town, that it either adjoined or was within eight feet of a range of houses occupied by some 300 individuals and was no more than sixty yards from the town centre. In the summer of 1847, the inhabitants of Killeshandra, County Cavan, threatened to pull down any fever shed that might be erected in the town, despite the fact that fever raged throughout the district. The temporary fever hospital at Fethard, County Tipperary, which had been opened in June 1847, was denounced from the altar on several occasions. The ambition of the parish priest and his curate, as they informed their flock repeatedly, was to see grass growing at the door of the hospital. One of their clerical harangues was delivered prior to the opening of a detached convalescence ward. Later that night, the building was maliciously burned to the ground. A similar arson attack had occurred in Belturbet, County Cavan, in April 1847.
Such extreme responses were prompted by fear of contagion, although, contrarily, the same fear prompted calls for the establishment of temporary fever hospitals, where the infected could be isolated. In all, 576 such applications were received by the central board of health, the authorising body, between February 1847 and August 1850, when the board was finally dissolved. Three hundred and seventy three of these were granted, the first at Tullamore, King’s County, on 26 February 1847, followed by Mitchelstown, County Cork, on 3 March. The last temporary fever hospital was established at Lisnaskea, County Fermanagh, on 17 October 1849. The weekly hospital returns demanded by the board of health showed that 332,462 patients were treated in these institutions from July 1847 to the disbandment of the service three years later. More females than males were accommodated, 173,723 as opposed to 158,739, but male mortality was higher. A total of 34,622 individuals died in the temporary hospitals, a death rate of 10.4 per cent. Despite the hostility that was levelled at these institutions, they alleviated suffering and saved lives. Given the sheer scale of the Famine, the failure of government to provide adequate financial support, and the relatively unadvanced state of contemporary medical practice, this was as much as could be expected of them.
Many doctors acknowledged their professional limitations and their inability to check the pestilence which raged around them. They were aware that dearth and disease were closely linked. They also knew that they did not have the antidote, that there was little they could do to counteract illness which originated in squalor and starvation. The political intervention they sought was overtaken by the natural. Famine-related death and emigration depleted the reservoir of disease in Ireland and the incidence of fever and other infectious diseases was significantly reduced in the wake of the disaster.
Laurence Geary is a Wellcome Research Fellow in the History of Medicine at the Royal College of Surgeons in Ireland
Further reading:
C. Poirtéir (ed.), The Great Irish Famine (Cork 1995).
R. Dudley Edwards and T. Desmond Williams (eds.), The Great Famine: Studies in Irish History, 1845-52 (Dublin 1956, 1994).
C. Morash and R. Hayes (eds.), Fearful Realities: New Perspectives on the Famine (Dublin forthcoming).
E. M. Crawford, Famine: the Irish Experience, 900-1900 (where? 1989)